Inherent Vascular Differences May Increase CVD Risk in Black Americans

Why are African Americans more prone to heart disease? While lifestyle factors such as diet and exercise obviously play a role, genetic differences in arterial function may offer another clue.
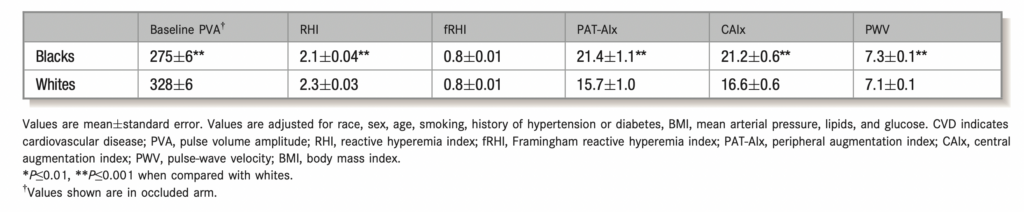
Black Americans are 30% more likely to suffer from heart disease compared to non-Hispanic whites, according to the CDC. And while socioeconomic and lifestyle factors invariably play a role, impaired vascular function may offer one other explanation why cardiovascular disease disproportionately affects Black Americans when compared with whites, researchers reported in the Journal of the American Heart Association. In the 2013 study, which involved 385 black and 470 white subjects, researchers used digital pulse amplitude tonometry (PAT) to measure reactive hyperemia index (or RHI, a measure of coronary endothelial dysfunction) and peripheral augmentation index (PAT-Alx). SphygmoCor applanation tonometry was then used to measure central augmentation index (C-Alx) and pulse wave velocity (PWV) to determine wave reflection and arterial stiffness. Even after adjusting for differences in CVD risk profiles, researchers found higher levels of arterial stiffness, greater wave reflection and more impaired endothelial function in black men compared with white. Significantly, these same results were reproduced in a sub-analysis of healthy black men. This study proves that inherent racial differences in vascular function may put black Americans at higher risk for CVD, independent of traditional CVD risk factors. Since poor arterial elasticity and weak endothelial function increase the likelihood of worse long term outcomes, the researchers concluded that non-invasive arterial analysis using digital vascular biomarkers are exceptionally useful tools for monitoring this high risk population.
Measures of Vascular Function by Racial Group Adjusted for CVD Risk Factors